Humanity’s Woes
I previously wrote about our son’s spirit, two days before his birth.
It was what my small brain could put together about motherhood & about being Carlos’ mom at the time.
It was at a time when the human him was going to be what I considered “typical”.
I haven’t brought myself to write again since October 24th because I had yet to be able to verbalize, put into sentences what has transpired since then.
What I want you to know before continuing to read is that I am using this piece as a form of therapy. There are so many what-ifs & so much guilt on my part as Carlos’ mother that I will have to work through for the foreseeable future.
Our beautiful Carlos Amado’s spirit embarked on its human journey on Monday, October 26th at 12:35 AM. It was the strange night in October when it snowed! The first of the many surprises we’d get that day.
In a lighter post, I’ll tell you about his birthday. Despite the difficulty & the fear that rushed over us that day, we had the most beautiful birth & from it came the most beautiful boy.
For this piece, I’d like to give light into what becoming parents of a medically complex kiddo looked like.
As soon as Amado was born, he was laid on my chest, as are most babies. We got to give the first kisses & feel his warmth, so excited for the world that we just entered as his parents.
He seemed so comfy, so content with where he was. He didn’t cry, which happens with some babies & I wasn’t surprised when his strong spirit came out in his strong self. But, the nurse got concerned after an extended period of time of no crying. It’s routine after a certain amount of time to get kiddos over to their bed & evaluate why they haven’t cried.
As I lay, numb & helpless, I asked Carlos over & over, “is he ok?” The doctors working on me: “he’s finnnne”.
Turns out, he wasn’t fine.
When he was transferred over to his bed, it took a lot to get Amado to cry. He eventually did but the nurses noticed that he wasn’t doing well swallowing the fluid in his mouth and, thus, not being able to breathe well enough to cry. During a whirlwind of noise & emotion, I was told that our son would be taken to the NICU for further evaluation & that they’d give us an update as soon as they had one.
In the matter of 20 minutes, I had given birth to our boy &, just like that, he was gone.
I had plans for skin to skin with me, with dad. Plans for counting fingers & toes. Plans for our first breastfeeding experience. Plans for Facetimes with his grandparents. Plans for waking up in the middle of the night to the realization that I had just given birth to a baby boy & smiling with joy.
Instead, it was several hours before we saw son again. When we did, we were told that he had to stay on his side or on his belly - he was struggling to breathe when on his back. We were told that there was concern about the size of his lower jaw & that his tongue may be impeding on his ability to breathe. The worry that went with the news wasn’t at the forefront of my mind. I wanted to be with my son.
That day was the start of the thought: “it’s just not fair”. It didn’t feel fair that I could hear other baby’s cry in the “mom & baby” rooms, while I had to go to the NICU to see our son. It didn’t feel fair that I had to ask a nurse if I could hold my son & I had to make sure wires weren’t pulling & that things were plugged in when I did hold my son. It didn’t feel fair that our first night together wouldn’t be together at all.
The deepest, most intense pain I’ve ever felt in my life was that night. We were told that our son’s condition couldn’t be treated there - he would have to be transferred to Children’s Mercy. We agreed, were grateful. Then, we were told that I couldn’t leave until the next day. Oh, yeah... My body just had a baby.
In the midst of processing what was going on with son, I had forgotten about myself. In a split second, all the pains came to me. The drained feeling. The literal pain in everything below my waist. The headache I still had from pushing (& probably from not sleeping). I came to the realization that I didn’t feel very well. & yet... I broke down at the thought that I couldn’t leave & be with my son.
I cried.
I cried every single time a nurse came in to check on me. I cried when the social worker came in to talk about Medicaid. I cried when we went downstairs to the cafeteria. I cried when the lactation nurse came to talk about how to use a pump instead of how to help my baby latch.
I asked when was the earliest I could leave. After being told the next day, I asked, “technically I can leave now though, right?” They couldn’t hold me hostage. They said yes, but they strongly suggested I didn’t. I thought about it. We knew it’d be best to know I was well first.
The next day, we woke up as soon as it was shift change. I was leaving ASAP & we were going to see our son. We left KU & headed straight to Children’s Mercy. No shower. No clothes change. No food.
When we got to Children’s Mercy, we were given more details about our son’s condition. The major complication was that his tongue was “falling” into his upper airway, making breathing through his mouth impossible - retrognathia. He was born with a lower jaw too small for his head - micrognathia - & since our tongues are attached to our lower jaws, his tongue was in his throat. We were given the instruction that he had to be on his side or belly at all times, as it was the only way he could breathe. At the time, I thought this was the solution. I didn’t consider that we’d need a long-term solution.
Typically, kiddos with this condition are considered for a distraction, where metal pieces are placed in the back of their jaw to push the jaw forward &, thus, move the tongue out of the airway. We did lots of research on mandibular distractions & it sounded like a “simple” fix & something that we could handle.
After his CT scan, we’d find out that he wasn’t a candidate.
I cried as the plastic surgeon told us that not only did our son have a jaw too small for him, it also came to a point at the front instead of being round. This meant that a mandibular distraction would only cause the bone to collide at the front, instead of being pushed forward (this is my explanation in simplest form - lots of words & explanations were given. The point was that he couldn’t get this surgery.)
In the same breath, the surgeon told us that our son would probably need a tracheostomy. I cried.
I was so embarrassed at how often I was crying. I cried to every nurse. Every doctor. I wish that as a society, we didn’t make moms feel embarrassment when crying after being told that their babies would need a life-saving surgery that would require needles, anesthesia, sedatives, narcotics, syringes, incisions - all in our baby’s tiny bodies.
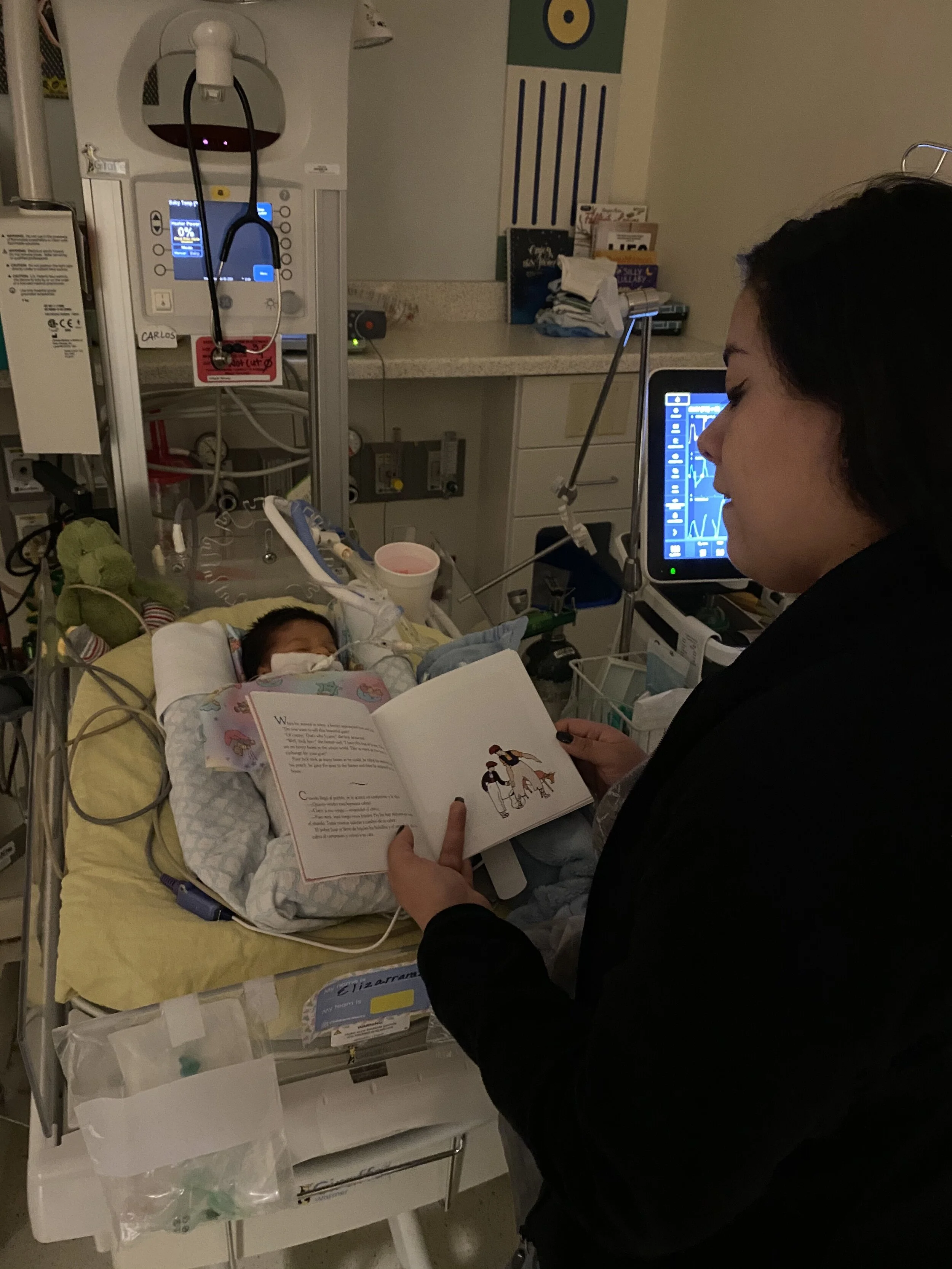
It took what seemed like an eternity for all of the doctors & nurses to coordinate a solid plan for our son. We were in the hospital for 2 weeks before the official decision was made to perform a tracheostomy on Amado. I found myself advocating & asking questions more than I would’ve liked.
I found myself having more of the responsibility to be logical & sane than I would’ve liked.
All at once I was: trying to understand all the medical terms & options, having to ask to hold my baby & having a nurse watch over these moments & make sure that he was in a position to breathe, mourning the fact that I had “missed out” on the typical newborn moments, oh, yeah, AND recovering physically from having just given birth. That on top of so much else.
Over the first few weeks, we’d have to live some of the most scary moments of our lives that I never wish on anybody - watching our son stop breathing. It happened 3-4 times over the 2 weeks before It was decided that son would need to be intubated. Watching our son stop breathing was the worst experience of my life. Watching him be intubated for a week is a close second.
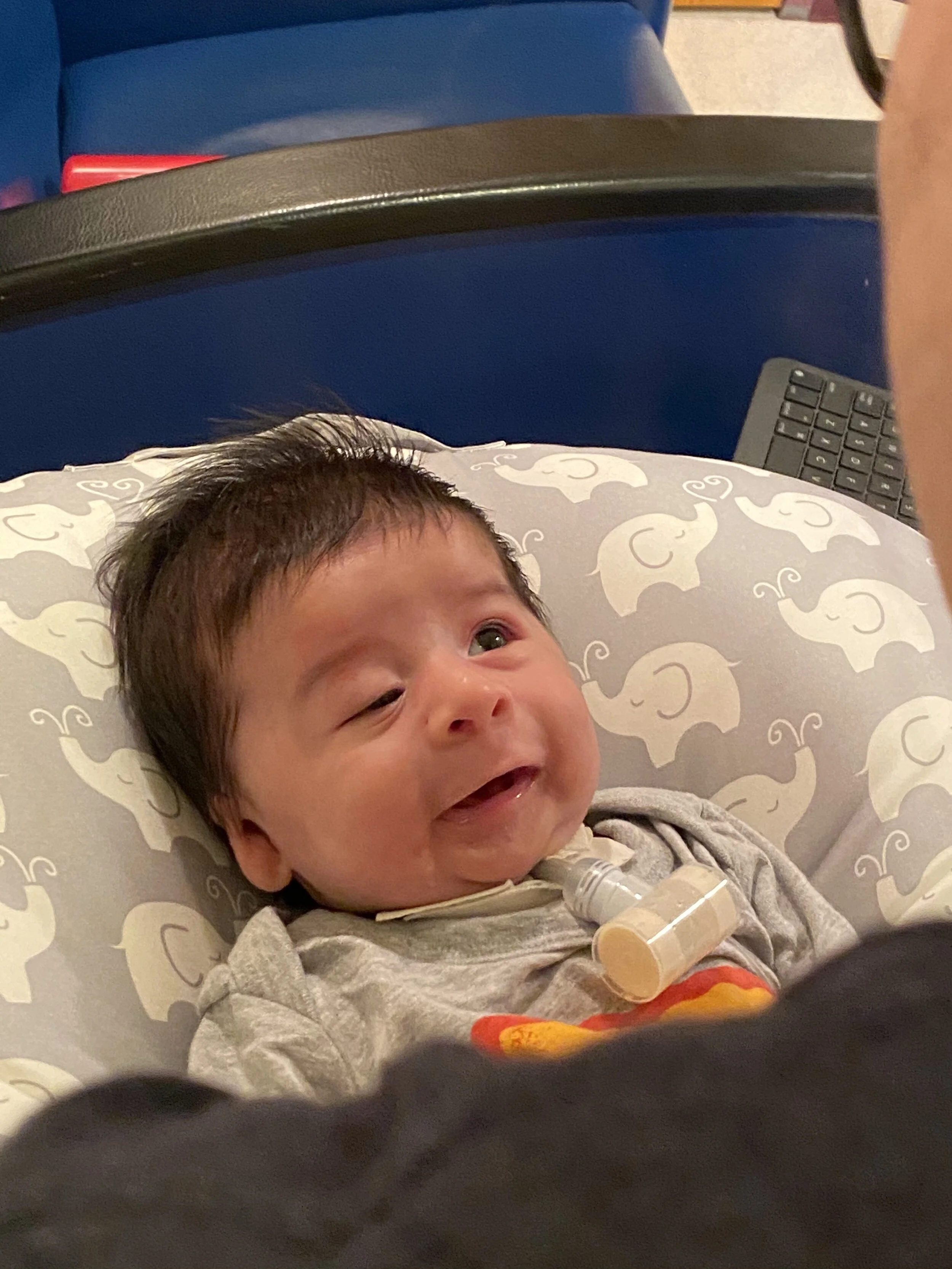
Looking back, I am so grateful, SO grateful that tracheostomies are an option. As much as we wanted the mandibular distraction & we had hoped that we could have this behind us sooner rather than later, seeing our son’s progress & seeing him thrive since his tracheostomy has been such a blessing.
Not having to worry about his position in order for him to breathe. Not leaving the hospital wondering if he’d stop breathing that night & if a nurse would be close enough to save his life. Not wondering if we’d ever have a life outside of a hospital. A tracheostomy made that happen for us, for Amado.
I mentioned guilt before.
Despite us knowing that a tracheostomy has been a God-send & how grateful we are for our son’s stability today, there are so many moments when we wonder “what-if” & those moments are immediately followed with the feeling of guilt.
I will use my blog to work through those emotions. I also look forward to sharing the many, many beautiful & inspiring moments that our Carlos Amado has brought into our lives. I cannot wait to tell you ALL about his strength & his goofiness & his hair & his love for his binky & his certainty about what he wants. Oh, yeah, & ALL about how his beautiful spirit shines through every single day.
Sana